Introduction
The nipple is a part of the nipple-areola complex (NAC) which is a specialized region of the breast with unique anatomical and histological characteristics.
The nipple-areola complex includes the nipple and the surrounding pigmented area called the areola. This complex can be affected by various conditions, including developmental abnormalities, benign processes like inflammation, infection, and tumours, and malignant diseases such as Paget’s disease and breast cancer. Clinical signs to watch for include skin changes, pathological nipple discharge, retraction, inversion, and palpable masses.
For a detailed evaluation, a multimodal imaging approach is often used, combining techniques like mammography, ultrasound, and MRI to accurately diagnose conditions affecting the nipple-areola complex.
The finding of discharge from the nipple of a nonlactating woman is a common condition.
It may be associated with an underlying carcinoma, albeit rarely.
Discharge from the nipple can occur from one or more lactiferous ducts.
Its management depends on:
- Presence of a lump (it should always be given priority),
- Presence of blood in the discharge or
- Discharge from a single duct or multiple ducts.
It is important to find out whether the discharge comes from one breast or from both breasts, or it comes from multiple ducts or from just one, and whether the discharge is clear or grossly bloody or blood tinged.
Types of Nipple Discharge: Normal vs Abnormal
Nipple Discharge may be either normal or abnormal.
In a parous woman a clear, serous discharge may be normal ( ‘physiological’).
It is often clear, yellow, brown, green, or white.
It usually comes from both breasts upon squeezing nipples.
Milky nipple discharge either spontaneous or on squeezing) is also normal (physiological) during pregnancy and breast feeding.
Abnormal Discharge is usually spontaneous and it occurs without squeezing the bereast.
It is caused by a disease or pathology in the breast.
It usually comes from one breast only, confined to a single duct, and is clear or blood-stained in appearance.
Other associated symptoms of an abnormal discharge are pain or a lump in the breast or ulceration or inversion of the nipple surface.
Purulent discharge suggests infection.
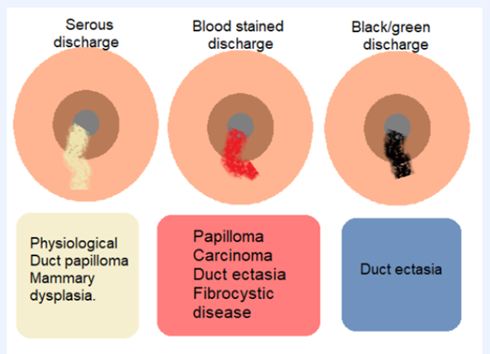
Nipple Discharge: Colour & Cause
Multiduct, multi-coloured discharge is usually physiological.
A blood-stained nipple discharge may indicate intraductal papilloma, intraductal carcinoma, duct ectasia, or fibrocystic disease.
A black or green nipple discharge is seen in duct ectasia.
Serous nipple discharge either clear or of any colour may be physiological or due to duct papilloma, mammary dysplasia, fibrocystic disease, duct ectasia or carcinoma.
Purulent nipple discharge indicates infection.
Milky nipple discharge occurs during lactation or rarely due to hypothyroidism and pituitary tumour such as prolactinoma.
Diagnosis of Nipple Discharge
A multimodal approach is used to evaluate nipple discharge.
Mammography and ultrasound can show underlying impalpable suspicious mass.
Cytological examination through FNAC may identify malignant cells, but a negative finding doesn’t rule out cancer.
Hemoglobin Test to detect the presence of blood in discharge fluid may be helpful.
Haemoglobin detected in nipple discharge may be secondary to an intraductal papilloma, intraductal carcinoma or duct ectasia.
Definitive diagnosis needs excisional biopsy of the involved duct and any associated mass lesion.
It is important to note, whether the discharge is coming from one breast or from both breasts.
Whether it comes from multiple duct orifices or from just one.
And whether the discharge is grossly bloody such as in trauma or blood stained in malignancy.
A milky discharge from both breasts in the absence of lactation or a history of recent lactation is called galactorrhea.
It may be associated with increased production of prolactin.
Radioimmunoassay for serum prolactin is diagnostic.
But True galactorrhea is rare.
KEY POINTS
The most common cause of spontaneous discharge from a single duct is a solitary intraductal papilloma (60%–80%).
MC cause of greenish discharge: Duct ectasia.
MC cause of blood-stained discharge: Duct papilloma.
Cancer is a very uncommon cause of discharge in the absence of other signs.
Nipple discharge associated with a cancer may be clear, bloody, or serous.
Papillomas located away from the nipple-areolar complex are at higher risk of malignancy (20%).
A papilloma is the most common benign tumor to develop breast cancer, mainly DCIS (Ductal Carcinoma in Situ).
Treatment options
Try to exclude first a carcinoma, by occult blood test and fine needle cytology.
Simple reassurance may be sufficient if no malignancy is suspected.
But if the discharge is causing a troublesome impact on lifestyle surgery can be done.
Two surgical procedures are microdochectomy and Hadfield Procedure.
Microdochectomy
In microdochectomy, the affected duct is excised through a tennis racquet incision or a periareolar incision.
Interestingly a papilloma is nearly always situated within 4–5 cm of the nipple orifice.
Hadfield Procedure
The Hadfield procedure or Cone Excision or Major Duct Excision is done when the location of the offending duct is uncertain or when there is bleeding or discharge from multiple ducts.
The entire major duct system is excised, and the specimen is sent for histopathological examination (HPE) without compromising the breast contour.
The complications of Hadfield operation are altered nipple sensation, nipple flattening or inversion and difficulty in breast feeding.

Leave a Reply